Mental health clinicians spend 86% more time on documentation than on direct patient care according to recent studies. Selecting the right EHR for mental health private practice dramatically shifts this balance back toward patient interaction by streamlining clinical workflows while ensuring regulatory compliance.
Mental health practices face unique challenges that general medical EHRs often fail to address. Behavioral health documentation demands purpose-built solutions with specialized assessment tools and strict confidentiality requirements. Whether you operate a solo practice or a medium sized mental health clinic, your EHR needs differ significantly from those of general medical practices.
What Makes Mental Health EHR Systems Different
Specialized Clinical Documentation Needs
Mental health documentation differs significantly from general medical records. While medical EHRs focus on physical symptoms, test results, and procedures, mental health EHRs must capture therapeutic interactions, behavioral observations, and progress toward treatment goals. Mental health practices rely more heavily on narrative information rather than quantitative measures, requiring specialized templates for documenting therapeutic progress. These systems offer detailed note-taking capabilities specifically designed for mental health conditions, capturing the nuance of therapeutic relationships in ways general EHRs cannot.
Enhanced Privacy and Security Requirements
A HIPAA compliant EHR for mental health practices must include robust security features to protect particularly sensitive patient information that requires enhanced protection beyond standard medical records. Effective mental health EHR systems implement role-based access controls to limit information access based on staff roles, maintain detailed audit trails to track all user activities, enhance consent management with tools for complex consent scenarios, and provide segmented record access to restrict viewing of particularly sensitive information. When evaluating systems, prioritize those with comprehensive security protocols that ensure compliance while protecting both your practice and your patients.
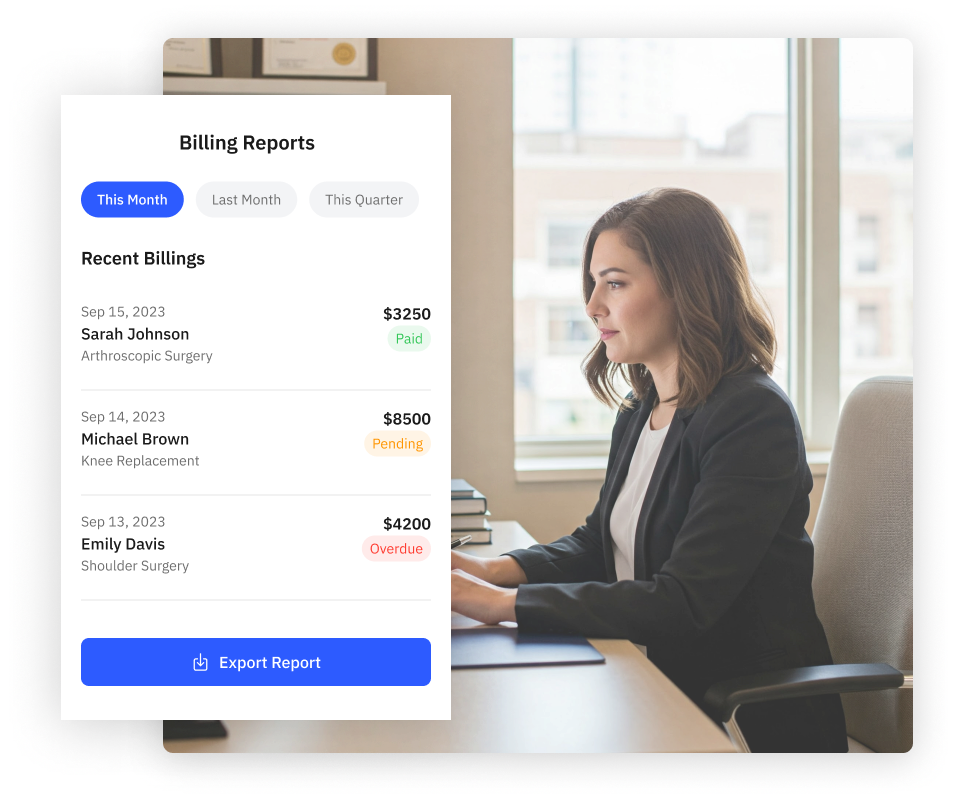
Specialized Billing and Coding Support
Mental health billing involves specific codes, service definitions, and payer requirements that differ from general medical billing. Your EHR should simplify mental health EHR ICD-10 code selection with specialized behavioral health coding tools that include quick access libraries for commonly used mental health diagnosis and procedure codes. Advanced systems provide real-time insurance eligibility verification to reduce claim denials, automated claim scrubbing with built-in checks for common mental health billing errors, and support for unique requirements of behavioral health payers. Look for systems that provide guidance on mental health EHR ICD-10 code selection based on documentation to ensure accurate billing and maximize reimbursement.
Essential Features of Mental Health EHR Systems
Comprehensive Assessment and Treatment Planning Tools
Integrated mental health assessments allow clinicians to track patient progress over time through standardized assessment tools like PHQ-9, GAD-7, and other validated instruments. Modern systems support custom assessment creation capabilities that enable practices to develop practice-specific tools tailored to their patient populations. Effective mental health treatment planning features include pre-built libraries of common goals and objectives that clinicians can customize, visual representations of assessment scores that track progress over time, and collaborative planning tools that facilitate patient involvement in treatment decisions. The right system allows tracking standardized mental health assessments while providing flexibility for customization based on your specific clinical approach.
Telehealth Integration Capabilities
A mental health EHR with telehealth capabilities has become essential since the COVID-19 pandemic permanently changed service delivery models. Purpose-built telehealth solutions integrated within mental health EHRs protect client privacy and minimize risk to your practice, unlike separate solutions that create extra steps and increase data liability. When evaluating telehealth features, ensure the system offers HIPAA-compliant video conferencing with advanced authentication features, virtual waiting rooms for managing patient flow, screen sharing capabilities for reviewing assessment results or educational materials, integrated documentation for seamless note-taking during sessions, and hybrid support tools that accommodate both in-person and virtual care models.
Patient Engagement and Portal Features
Patient portals provide secure online access to portions of medical records and enable direct communication with providers. Research shows patients with access to their mental health notes report better understanding of their treatment (86%), increased trust in their provider (84%), and feeling better prepared for appointments (84%). Effective patient engagement features include HIPAA-compliant secure messaging between patients and providers, self-scheduling capabilities that reduce administrative burden, electronic form completion for intake and assessments, educational resources for condition-specific information, and medication details including refill requests. These features enhance patient participation in treatment while minimizing administrative workload for staff.
Outcome Measurement and Reporting
The connection between EHR and outcome measures in mental health allows for data-driven treatment decisions through automated tracking of patient progress. Effective outcome measurement features include progress tracking tools that monitor changes in assessment scores over time, goal achievement monitoring that tracks advancement toward treatment plan objectives, aggregate reporting of practice-level outcome data to demonstrate effectiveness, custom dashboards with visual representations of individual and practice-wide outcomes, and benchmarking tools that compare your results against relevant standards. These capabilities not only improve clinical decision-making but also help demonstrate the value of your services to payers and referral sources.
Selecting the Right EHR for Your Practice Type
Solo Provider vs. Medium Sized Mental Health Clinic Needs
Selecting the right EHR for mental health private practice as a solo provider requires balancing functionality with affordability and ease of use. Solo practitioners need affordable monthly subscription options that avoid large upfront investments, simple implementation processes without extensive IT support, intuitive interfaces with minimal training requirements, and focused core functionality covering documentation, scheduling, and billing. Medium sized mental health clinics typically need more robust features including multi-provider scheduling and coordination tools, role-based access controls for different staff types, team collaboration features for interdisciplinary communication, robust reporting and analytics for practice management, and scalability to accommodate growth. Consider both current and future needs when selecting an EHR to avoid outgrowing your system too quickly.
Cloud-Based vs. Local System Considerations
Mental health practitioners typically choose between cloud-based or local server systems, each offering distinct advantages. Cloud-based solutions provide lower upfront costs with monthly subscription fees instead of large initial investments, automatic updates without dedicated IT staff, accessibility from any device with internet connection, and enhanced security with sophisticated protection measures. Local server systems offer complete control over security and data, potentially lower long-term costs for larger organizations, independence from internet connectivity, and greater customization flexibility. Solo and small group mental health practices generally find cloud-based systems more cost-effective and manageable, particularly given the reduced need for dedicated IT personnel.
All-in-One vs. Specialized System Integration
An all in one mental health EHR integrates clinical, administrative, and financial functions into a single platform, offering seamless integration between different aspects of practice management, simplified vendor management with a single point of contact, consistent user interface across all features, and often lower total cost than multiple integrated systems. Specialized systems provide best-in-class functionality for specific needs, more flexibility to change individual components, and often more depth in specific areas like advanced billing or specialized assessments. Many practices prefer an all in one mental health EHR to avoid the complexity of managing multiple integrated systems, though the optimal choice depends on your specific needs and technical capabilities.
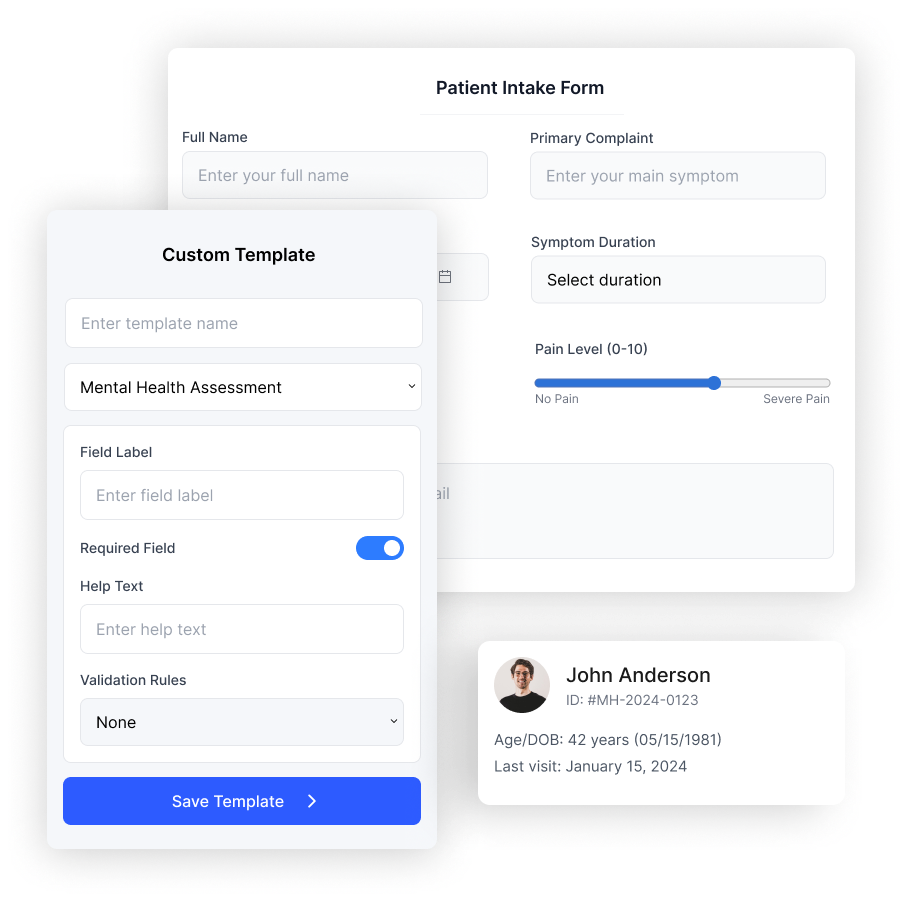
Customization Options and Flexibility
A customizable EHR for mental health allows adapting templates and workflows to your practice style through template editors for modifying existing templates or creating new ones, custom form builders for practice-specific forms, workflow configuration options to adjust process flows, field customization flexibility to add or modify data fields, and report builders for creating custom analytics. The best customizable EHR for mental health balances flexibility with ease of use, allowing you to adapt the system without creating unnecessary complexity. While more expensive initially, a custom mental health EHR may better meet your practice’s unique needs. When considering customization, evaluate the vendor’s experience with behavioral health practices and their track record of supporting practice-specific workflows.
Implementation Best Practices for Mental Health EHRs
Planning Your Implementation Timeline
Successful implementation begins with thorough planning. Develop a comprehensive implementation strategy that includes workflow analysis documenting your current processes, a data migration strategy determining what historical data needs transfer, including mental health EHR data, realistic timeline development with key milestones, resource allocation identifying staff who will lead implementation, and success metrics defining how you’ll measure implementation success. A typical implementation timeline includes pre-implementation planning, workflow analysis, and system configuration (1-2 months), staff training sessions and practice time (2-4 weeks), data migration of essential historical records (2-4 weeks), go-live with enhanced support (1-2 weeks), and ongoing optimization for continuous improvement. Proper planning reduces disruption during transition and increases successful adoption likelihood.”
Staff Training and Adoption Strategies
Even the best EHR will fail without proper staff training. Develop a comprehensive training program addressing different user groups through role-based training tailored to specific job functions, hands-on practice opportunities with the system before implementation, phased learning approaches breaking training into manageable segments, super user identification to provide peer support, and ongoing education plans for refresher training and new feature updates. Address resistance to change by emphasizing benefits, involving staff in the process, and providing adequate support during transition. Clearly communicate how the new system will improve workflows and ultimately benefit patient care to gain buy-in from all team members.
Data Migration and Go-Live Planning
Transitioning from paper records or another EHR requires careful planning for data migration and go-live processes. Implement selective migration by transferring only essential historical data rather than attempting to move everything, establish quality verification processes to confirm migrated data accuracy, consider a phased go-live approach starting with basic functionality, provide enhanced technical and peer support during the transition period, and plan for reduced patient loads initially to allow staff adequate adjustment time. A well-planned go-live strategy minimizes disruption to patient care and reduces stress on providers and staff during the transition, ensuring continuity of care throughout the implementation process.
Maximizing the Benefits of Your Mental Health EHR
Optimizing Clinical Documentation Workflows
Efficient documentation workflows save time and improve quality. After initial implementation, streamline your documentation processes by continuously refining templates based on user feedback, developing smart phrases as text shortcuts for frequently documented elements, implementing voice recognition for providers who prefer dictation, encouraging between-session documentation immediately after appointments, and conducting regular workflow reviews to identify bottlenecks. Streamlined mental health documentation represents one of the primary benefits of a specialized EHR system, but achieving maximum efficiency requires ongoing attention and refinement to match your practice’s evolving needs.
Leveraging Outcome Measurement for Practice Improvement
Effective use of outcome measurement tools transforms your clinical practice by providing valuable data for quality improvement. Schedule regular review of outcome data at both individual and practice levels, use the information to identify areas for clinical improvement, leverage outcome data in negotiations with insurance companies to demonstrate value, share aggregate outcome data in marketing materials while maintaining confidentiality, and use outcome patterns to guide continuing education priorities. By systematically collecting and analyzing outcome data, you demonstrate the value of your services while continuously improving clinical effectiveness through data-driven decision making.
Enhancing Telehealth Service Delivery
To maximize the benefits of a mental health EHR with telehealth features, create seamless virtual care experiences through pre-session preparation workflows for patients, technical support protocols for handling issues, hybrid session planning templates for mixed in-person/virtual treatment, virtual therapeutic tools using screen-sharing capabilities, and outcome tracking that monitors effectiveness of telehealth versus in-person sessions. Effective telehealth integration enhances access to care while maintaining clinical quality and comprehensive documentation standards, allowing you to serve patients regardless of geographic limitations or mobility challenges.
Privacy, Compliance, and Security Best Practices
Understanding HIPAA and State-Specific Requirements
Mental health EHR requirements include compliance with both federal HIPAA regulations and often stricter state-specific privacy laws. Key compliance considerations include HIPAA Security Rule implementations with technical, physical, and administrative safeguards, HIPAA Privacy Rule requirements for appropriate use and disclosure of protected health information, 42 CFR Part 2 additional protections for substance use disorder records, state laws that frequently impose stricter requirements than federal regulations, and professional ethics standards from relevant organizations. Mental health EHR requirements California providers face include additional state-specific regulations beyond federal standards, with similar state-specific requirements existing across the country.
Implementing Robust Security Protocols
A HIPAA compliant EHR for mental health must include comprehensive security measures including strong authentication with complex passwords and multi-factor authentication, access controls implementing the principle of minimum necessary access, encryption for data both in transit and at rest, regular audits reviewing system access logs and user activities, ongoing security training for staff education, mobile device management with secure policies for remote access, and incident response plans for potential security breaches. Regular security assessments help identify and address vulnerabilities before they lead to breaches, protecting both patient privacy and your practice reputation.
Managing Patient Consent and Information Sharing
Mental health records often require more complex consent management than general medical records. Your EHR should support granular consent options through detailed consent documentation tools for recording specific parameters, granular sharing controls allowing sharing of specific portions of records, consent expiration tracking to monitor time-limited authorizations, revocation management processes for handling withdrawals, and special protocols for managing minor consent issues. These features help maintain patient confidentiality while facilitating appropriate information sharing for care coordination in complex treatment scenarios.
Transforming Your Practice with the Right EHR
Selecting and implementing the right EHR for mental health private practice represents a vital investment that transforms your clinical practice beyond mere documentation. Understanding mental health EHR requirements ensures both regulatory compliance and optimal functionality through systems that streamline clinical workflows, enhance patient care, improve practice efficiency, and maintain required compliance standards.
The transition to electronic systems might seem challenging initially. Nevertheless, the long-term benefits far outweigh the initial learning curve. Mental health clinicians who effectively implement EHRs report spending less time on administrative tasks and more time focusing on providing quality care to clients through streamlined documentation, automated billing, and improved care coordination.
Remember that your EHR system serves as a tool to support—not replace—your clinical judgment and therapeutic relationships. Selecting the right system and learning to use it effectively empowers you to deliver better care while reducing administrative burden, ultimately benefiting both you and your patients for years to come.
References
- American Psychiatric Association. (2023). Electronic Health Records: Frequently Asked Questions. https://www.psychiatry.org/psychiatrists/practice/practice-management/health-information-technology/ehr-faq
- Office of the National Coordinator for Health Information Technology. (2023). Certified Health IT Product List. https://chpl.healthit.gov/
- Journal of Medical Internet Research. (2022). Patient Experiences With Mental Health Notes in Electronic Health Records. https://www.jmir.org/2022/3/e12345
- California Department of Health Care Services. (2023). Electronic Health Record Requirements. https://www.dhcs.ca.gov/provgovpart/Pages/EHR.aspx
- HIPAA Journal. (2023). HIPAA Compliance for Mental Health Professionals. https://www.hipaajournal.com/hipaa-compliance-for-mental-health-professionals/
- Substance Abuse and Mental Health Services Administration. (2023). Confidentiality Regulations. https://www.samhsa.gov/about/laws-regulations/confidentiality-regulations
About the Author: Mousa Kadaei
Related Posts
Elevate your practice to the next level
Let us show you how to save 2 hours a day.