When you discover how key electronic health records are, your view on healthcare shifts and loads of medical setups these days are all about EHRs to improve patient experience. The right use of these records means doctors and patients get to benefit from being safe and having simple ways to get to info. Electronic health records bring a bunch of good stuff to the table but let’s not forget that they’ve got their downsides, too. When rolling these systems out, you gotta weigh the advantages of electronic health records against the disadvantages of electronic health records.
What are electronic health records?
Just so we’re clear, an “electronic health record system” is the digital version of a patient’s paper chart. EHRs focus on the individual offering up-to-the-minute records accessible by authorized folks. Plus, they’re not just about keeping track of treatments and medical histories. They give the full scoop on a patient’s health details. Now why are EHRs so big-deal important? Let’s dive into that.
Electronic Health Records focus on saving data . These patient records get regular updates. Also, EHRs are available to those with permission. Inside, you’ll find thorough medical histories, medicines, X-ray images, allergies, and test outcomes. So, these records support healthcare pros in choosing the best care steps. Through data analytics, electronic health records promote better care and assist in reducing costs.
Check out these articles after you’re done
Benefits of electronic health records in healthcare
Discussing the value of electronic health records, we gotta spotlight the “electronic health records benefits” in the medical world. These EHRs give docs a hand with patient care and notch up the healthcare game cause they:
- Ensure the patient’s health information is spot on, boosting the precise-ness of the data.
- Swiftly pull up patient histories for care that are better synchronized and go smoother.
- Boost how much work healthcare pros can get done and help them have a better time away from the job.
- Make prescribing more secure and reliable with systems like computerized physician order entry.
- Assist healthcare experts in figuring out what’s up with patients, cutting down on goof-ups, and making treatment less dicey.
- Enhance the chat between patients and health workers.
- Keep patient info private and safe from prying eyes.
- Slash expenses by cutting out paperwork, beefing up safety, avoiding repeat tests, and promoting top-notch health.
The biggest perk of this organized info is its shareability with other medical pros in various health outfits via health information exchange. EHR data setups let you pass details to drug stores, test centers, picture scan places, expert docs, and the like.
Difference between EHR and EMR
You’ve got the hang of how vital electronic health records are. Alright, let’s get down to what makes EMR different from EHR. I’ve got your back; we’re gonna break it down real simple! But first up, we gotta nail down what an EMR is.
Generally, What is an EMR? An electronic medical record is an electronic version of a medical chart. With EMR, a patient’s history doesn’t travel easily outside the practice. Furthermore, EMRs are usually used by providers for treatment and diagnosis.
As to the differences in usage trends between EHR and EMRs, EHRs are more advanced. First, EHRs will be the healthcare system’s future due to the holistic coordination within the healthcare ecosystem. The truth is that the term EHR is now referenced more systematically. Not to mention that EHR systems exceed essential functions like documentation and clinical notes. It includes the practice workflows from a broader perspective, integrating other parties in the healthcare system.
Boosting teamwork in healthcare settings, EHR systems also ramp up how much patients get involved. Plus, they better patient care quality. All that and it even makes a practice more cost-effective and efficient. Wanna get the lowdown on why EHR should grab your focus?
How has the EMR changed the workflow in healthcare systems
Electronic Medical Records also known as EMRs, have shaken things up in healthcare. They’ve changed the game on how we keep track of patient stuff and who can see it. Now, we’ve got all this patient info saved as “digital medical records.” Anyone can get to it if they have a computer or phone and can get into the system making things run smoother for the medical teams and making “clinical workflows” work better.
Thanks to EMRs, docs and other medical pros can get a patient’s details super fast and make smart choices for their health. They can pull up all the copies of a patient’s records so everyone knows the latest on the patient’s past health stuff, what meds they’re on, and what their tests are saying. This is a big deal when a bunch of different medical folks are trying to help the same patient.
Algorithms and simple rules that analyze patient info and dish out advice to health pros based on “evidence-based guidelines” represent another trick up EMR’s sleeve that’s overhauling healthcare system workflows. This tweak’s making sure we get the diagnosis and care plans spot-on, which means patients get the best treatment possible.
Tracking patient results and keeping an eye on care quality has gotten heaps easier with EMRs. Health systems now have an easy time gathering info on how patients are doing, and they can spot the bits where things could be better. This leads to sharper treatment strategies cooler patient experiences, and a smarter way to use resources.
Why do we gotta have EHRs if we wanna see healthcare get better?
EHRs come in real handy for boosting the healthcare scene, right? They give docs a super detailed rundown of a person’s health history. All that info gets passed around to different healthcare pros, which means they get the full picture and can work together better. They even get to see stuff like what meds someone’s on or their lab work straight away.
This means when it comes to making choices about someone’s care, they’ve got all the deets they need. Plus, with EHRs, there’s less chance a doc will mess up and give you the wrong pills or treatment because they’ve got your past health stuff and meds at their fingertips. And say you’re allergic to some drug or another, EHRs can wave a red flag so everybody knows. That’s a big win for keeping patients safe.
Healthcare professionals can track and keep an eye on patient data over time with EHRs, which helps to manage population health and “chronic disease management.” They use this info to spot folks who might get sick and give care before things get worse. Doing this might lower the number of hospital stays and stop more serious health problems.
Mandatory use of EMR/EHR in healthcare
The 2009 American Recovery and Reinvestment Act encouraged doctors to start using Electronic Medical Records (EMRs) to make patient care better and safer. Lots of hospitals and clinics picked up EMRs because of this, and some places even require them now.
Some folks don’t like that EMRs have to be used everywhere. They say smaller clinics might find it too expensive and it could mean less time with patients. Getting an EMR going costs a lot of effort and cash, and it shakes up how doctors do their thing. Plus, people worry that keeping patient details on computers might not be safe or private enough.
Even with these worries, the push for required EMR adoption in the medical field seems set to carry on. With tech getting better and cheaper, it’s simpler now for places that treat sick people, no matter their size, to bring in EMRs. The pluses of EMRs, like bettering patient safety and work flow, are tough to overlook. Lots of doctors and nurses are already diggin’ the good things these systems bring.
How much money did healthcare invest in EHRs?
Over the last ten years, the healthcare sector has poured a hefty sum into EHRs (electronic health records) setup. An Office of the National Coordinator for Health Information Technology (ONC) publication mentions that since the 2009 HITECH (Health Information Technology for Economic and Clinical Health) Act, US hospitals have dropped over $30 billion just to get EHRs up and running.
The HITECH Act offered financial perks to healthcare pros to encourage them to adopt EHR technology. This push is why we’ve seen such a bump in EHR use in the last ten years. In addition to those bucks, the bigwigs at the Centers for Medicare and Medicaid Services rolled out the EHR Incentive Programs. These programs offered extra rewards to doctors who mastered using EHR technology the way they should—you know, the “meaningful use” certified stuff.
Dropping cash on EHRs at the start wasn’t a small change, and that’s the real talk. But here’s the scoop – the long haul is looking bright. We’re talking about better patient health wins, not spending an arm and a leg on healthcare, and making sure everyone involved in the care game is on the same page. Those goodies should make the first dent in the wallet feel like chump change later on.
Which EMR/EHR system is mainly implemented in healthcare
There are many different electronic medical record (EMR) systems in healthcare, and the most implemented system can vary depending on the region, type of healthcare organization, and other factors. However, according to a 2021 report from KLAS Research, the top three most implemented EMR systems in the United States are:
Epic Systems: Epic is a widely used EMR system in large hospitals and health systems across the United States. Epic is known for its interoperability features, allowing healthcare organizations to share patient data securely.
Cerner Corporation: Cerner is another widely used EMR system in mid-size and large hospitals. Cerner’s system is known for its customizable workflows and real-time data analysis capabilities.
Meditech: Meditech is a long-standing EMR system that has been in use for over 50 years. It is trendy among smaller hospitals and healthcare organizations. Meditech’s system is known for its user-friendly interface and easy implementation.
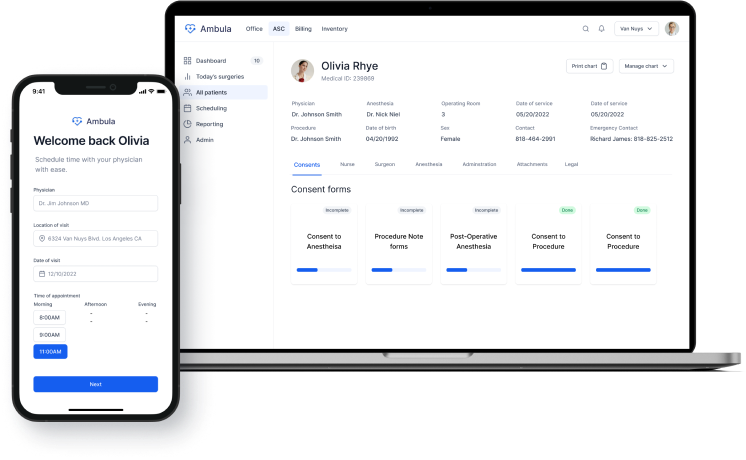
Ambula EMR: Ambula is one of the more modern implementations of EMR systems in healthcare. It is designed for outpatient settings, offering appointment scheduling, patient registration, electronic prescribing, and charting features. Many ambulatory care clinics, surgery centers, and physician practices across the United States use it.
Improved Public Health
One of the key contributions of EHRs to public health is their ability to enhance disease surveillance. By tracking the occurrence of reportable diseases and conditions, EHRs can provide real-time data on the spread of diseases and identify outbreaks early on. This timely information allows public health officials to take prompt action to contain outbreaks and prevent the spread of diseases. For instance, EHR data can be used to monitor the prevalence of influenza and identify areas where vaccination rates are low, enabling targeted interventions to improve immunization coverage.
EHRs also facilitate outbreak investigations by providing a centralized repository of patient information. This includes data on patient demographics, medical history, clinical presentation, laboratory results, and treatment outcomes. By analyzing this data, public health officials can identify the source of an outbreak, determine the mode of transmission, and develop effective control measures. For example, EHR data can be used to trace the spread of a foodborne illness by identifying the common food item consumed by affected individuals.
Better care?
On the same note, not only do EHRs offer better care, they automate a lot of tasks. Besides, EHRs ensure doctors can exchange data remotely with updated accuracy. Furthermore, they are customizable according to each case and flexible by nature. The main advantages of electronic health record software include a higher quality of care. While EHR provides easy and quick access to records, it increases the practice’s efficiency. They offer a more successful medical approach because they help recognize patterns, predict the diagnosis, and offer possible treatments. Both patients and physicians benefit from this tracking analytical device. Here’s how EHR enhances the care quality experience.
- A study published in the journal JAMA Internal Medicine in 2023 found that EHRs can reduce medication errors by up to 80%. The study looked at data from over 100 hospitals and found that hospitals with EHRs had significantly lower rates of medication errors than hospitals without EHRs.
- Another study, published in Health Affairs in 2023, found that EHRs can improve patient care coordination. The study looked at data from over 10,000 patients and found that patients whose care was coordinated through an EHR had better outcomes than patients who did not.
- A third study, published in The Lancet in 2023, found that EHRs can improve patient safety. The study looked at data from over 1 million patients and found that patients who received care in hospitals with EHRs had lower rates of adverse events than those without EHRs.
Here’s a deeper look into the perspectives of healthcare professionals on the importance of EHRs:
Dr. Lloyd Minor of Stanford Medicine emphasizes the transformative role of EHRs in healthcare. He mentions, “Electronic health records are foundational to the digital revolution in healthcare, playing a critical role in achieving better health outcomes and more cost-effective care.” This indicates that EHRs are not just about digitizing patient records but also about improving the efficiency and effectiveness of healthcare delivery.
Improved Clinical Decision Support
Clinical decision support systems leverage a range of data sources, including electronic health records (EHRs), clinical guidelines, and real-time patient data, to provide clinicians with timely and relevant recommendations at the point of care.
One of the primary benefits of improved CDS is its ability to reduce medication errors. By providing real-time alerts and warnings about potential drug interactions, contraindications, and dosing errors, CDS systems can help prevent adverse drug events (ADEs), which are a significant cause of patient harm. A study published in the Journal of the American Medical Association found that CDS systems can reduce medication errors by up to 50%.
In addition to reducing medication errors, CDS systems can improve the quality and appropriateness of care by providing clinicians with evidence-based treatment, diagnosis, and preventive care recommendations. These recommendations are based on the latest clinical guidelines and research, ensuring patients receive the most up-to-date and effective care. A study published in the journal Annals of Internal Medicine found that CDS systems can increase adherence to clinical guidelines by up to 20%.
Future of EMR in Healthcare
The future of electronic medical records (EMRs) in healthcare is exciting and promising. As technology advances, EMRs will become more sophisticated, streamlined, and integrated with other healthcare systems. One of the most significant benefits of EMRs is that they allow easy access to patient records across different healthcare settings. This interoperability will become even more seamless in the future, allowing for real-time data exchange and improved care coordination.
The future of EMRs in healthcare will also focus on improving the user experience for healthcare providers. EMRs will become more intuitive and user-friendly, reducing the documentation burden and allowing providers to spend more time on patient care. Furthermore, EMRs will continue to evolve to include more patient-generated data, such as wearable devices, to provide a complete picture of a patient’s health.
Finally, if you have any questions or need to know more about EHR systems, the Ambula team is always ready to help! Contact us at: (818) 308-4108! And now, paper charting vs. electronic charting: which one is better?