What does ROI stand for in healthcare?
In healthcare, ROI stands for Return on Investment. It measures the financial benefits gained from investments in healthcare systems, such as Electronic Health Records (EHR), relative to the costs incurred. ROI is a critical metric used to evaluate the efficiency and profitability of healthcare investments by comparing the gains from improved patient care, operational efficiency, and reduced errors against the expenses of implementing and maintaining these systems.
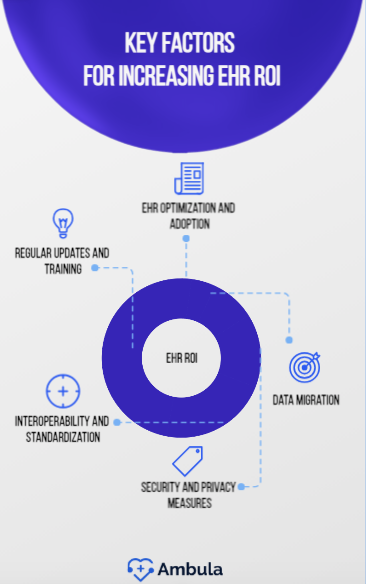
This blog post will provide insights on how to maximize your EHR ROI. We will cover different strategies like EHR optimization, consistent training, regular updates, and the role of qualitative metrics. We will also delve into enhanced care quality, reduced readmissions, document standardization and interoperability, physician satisfaction, technical expertise, usability, privacy, security, and the significance of successful data migration.
EHR Optimization: A Definitive Overview
Definition: EHR Optimization refers to the systematic process of refining and enhancing an Electronic Health Records (EHR) system to better align with healthcare providers’ specific needs and workflows. It encompasses a range of activities, from software customization and user training to hardware upgrades and data management improvements.
Significance: The importance of EHR Optimization cannot be overstated. As healthcare becomes increasingly digitized, the efficiency and effectiveness of EHR systems play a pivotal role in patient care and operational success. Here’s why EHR Optimization is paramount:
- Enhanced Patient Care: An optimized EHR system ensures that clinicians have quick and accurate access to patient data, enabling better decision-making and improved patient outcomes.
- Operational Efficiency: Streamlined workflows, reduced data entry errors, and faster access to records mean healthcare providers can see more patients and reduce administrative burdens.
- Financial Benefits: By eliminating inefficiencies and reducing errors, healthcare organizations can save costs and improve their return on investment in EHR systems.
- User Satisfaction: A system tailored to the needs of its users reduces frustration and burnout among clinicians, leading to higher job satisfaction and better patient interactions.
- Future-Proofing: As healthcare regulations and technologies evolve, an optimized EHR system can adapt more easily, ensuring that healthcare providers remain compliant and at the forefront of patient care innovation.
In essence, EHR Optimization is not just a technical endeavor but a strategic imperative for healthcare organizations aiming for excellence in a digital age.
How to measure EHR ROI?
Measuring EHR ROI involves evaluating a combination of financial and non-financial metrics. Start by tracking cost savings, which include reductions in paper use, storage needs, and administrative expenses. Also, the financial impact of fewer medical errors and redundant tests, which can significantly lower costs, should be considered.
Next, revenue increases can be assessed by examining improvements in billing accuracy, faster claims processing, and potentially higher patient volumes due to enhanced service efficiency. Operational efficiency gains should be measured by the time saved for staff, and smoother patient flows, and reduced appointment no-show rates.
Strategies for EHR Optimization
EHR Optimization and Adoption
The phase of EHR adoption goes beyond using a digital platform to store health records. It’s about optimally aligning the EHR technology with the practice’s unique needs to increase operational efficiency, reduce costs, and improve the quality of care. Therefore, EHR Optimization is a continuous process that goes hand in hand with EHR Adoption.
Firstly, the EHR adoption phase must be carefully strategized. It’s crucial to invest enough time in selecting an EHR system that best suits your practice’s needs, focusing on usability and scalability. Customization can also make the system more attuned to your specific requirements.
Post-implementation, the optimization phase works on continuously making adjustments for improvements. Regular feedback cycles from users can help make small, incremental changes that improve the system’s overall effectiveness. Additionally, a thorough review of workflow processes can identify areas of improvement, leading to increased efficiencies.
Regular Updates and Training
Keeping your EHR system updated with the latest features and enhancements is crucial for maintaining its efficacy. Regular updates not only ensure security but also introduce new features that help in enhancing operational efficiency. It’s important to engage with your EHR vendors to keep abreast of the latest updates and security patches.
However, regular updates alone are not enough. Training the users on the system’s functions and new features is equally important. Regular training sessions ensure that all users are proficient at using the system, reducing on-the-job learning time, minimizing errors, and increasing productivity.
Training should also include cybersecurity awareness, as healthcare data is a prime target for cyber attacks. Ensuring your team understands how to use and manage patients’ health information safely can enhance security and privacy.
Monitoring Qualitative Metrics and Enhanced Care Quality
Monitoring qualitative metrics is an important method to evaluate the effectiveness of your EHR system. Metrics can help you assess user satisfaction, time efficiency, patient outcomes, and other critical indices. Closely monitoring these performance indicators can provide valuable insight into areas that require attention and improvement, thereby contributing to continuous EHR optimization.
Concomitantly, a well-optimized EHR system translates into enhanced quality of care. By having easy access to comprehensive patient data, physicians can make more accurate diagnoses and provide more personalized care to their patients. Additionally, better coordination and interoperability between different healthcare providers reduce the risk of duplicative tests or treatments, reducing costs and increasing patient satisfaction.
Achieving Break-Even Point
The break-even point is a critical milestone when cost savings equals the investment made on EHR. It’s essential to determine when this point will be reached and devise a strategy to reach it as quickly as possible. This requires thorough cost and benefit analyses and careful financial planning pre- and post-EHR implementation.
There are proven ways of accelerating the time taken to reach the break-even point. These include focusing on strategies that increase revenue (like maximizing patient throughput or offering additional billable services) and lowering expenses (like reducing medical errors and minimizing duplicate tests).
Case Studies
There are many case studies of healthcare providers who have successfully obtained a high ROI from their EHR systems. They have used various strategies mentioned above, like careful adoption, regular updates and training, importance given to interoperability and standardization, and so on. Studying these cases is hugely beneficial as they serve as a repository of practical knowledge to help devise your EHR strategy.
- Stanford Medicine: Stanford Medicine implemented an EHR system in 2011. The system has helped the organization improve patient care, reduce costs, and improve the efficiency of its operations. Stanford Medicine has estimated that the EHR system has saved the organization $1 billion over the past 10 years.
- Kaiser Permanente: Kaiser Permanente is a large integrated healthcare delivery system that implemented an EHR system in 2009. The system has helped Kaiser Permanente improve patient care, reduce costs, and improve the efficiency of its operations. Kaiser Permanente has estimated that the EHR system has saved the organization $1.7 billion over the past 10 years.
- Intermountain Healthcare: Intermountain Healthcare is a large healthcare system that implemented an EHR system in 2006. The system has helped Intermountain Healthcare improve patient care, reduce costs, and improve the efficiency of its operations. Intermountain Healthcare has estimated that the EHR system has saved the organization $2 billion over the past 10 years.
- Mayo Clinic: Mayo Clinic is a large academic medical center that implemented an EHR system in 2010. The system has helped Mayo Clinic improve patient care, reduce costs, and improve the efficiency of its operations. Mayo Clinic has estimated that the EHR system has saved the organization $1.5 billion over the past 10 years.
Technological Aspects of EHR Optimization
EHR Optimization is not solely about refining the user interface or improving workflows; it’s deeply rooted in the technological foundations of the system. Here’s a breakdown of the technological aspects integral to EHR Optimization:
- Hardware Infrastructure: The physical servers, computers, and network systems on which the EHR runs play a crucial role. Ensuring these are up-to-date, fast, and reliable is essential. For instance, slow server speeds can cause delays in accessing patient records.
- Software Updates: Regularly updating the EHR software ensures the system benefits from the latest features, security patches, and bug fixes. An outdated system can have vulnerabilities and may not offer the latest functionalities.
- Data Security and Compliance: With the increasing cyber-attack threat, securing the EHR system is paramount. This includes encryption protocols, regular security audits, and adherence to regulations like HIPAA.
- Interoperability: One of the significant challenges in modern healthcare is ensuring different systems can communicate seamlessly. Technological solutions that promote interoperability allow EHR systems to exchange data with other healthcare technologies, ensuring a unified view of patient information.
- Cloud Integration: Many modern EHR systems are moving to the cloud, offering benefits like remote access, scalability, and reduced on-premise infrastructure costs. However, this transition needs to be managed with security and data integrity considerations.
- User Interface and Experience: The design and usability of the EHR system play a significant role in its effectiveness. Technological enhancements can simplify complex tasks, reduce the number of clicks, and make the system more intuitive for users.
- Backup and Disaster Recovery: Technological measures need to be in place to ensure data is regularly backed up and can be quickly restored in case of system failures or other unforeseen events.
- Analytics and Reporting: Integrating advanced analytics tools can help healthcare providers derive insights from the vast amounts of data in EHR systems, aiding in decision-making and improving patient care.
In summary, the technological aspects of EHR Optimization encompass a holistic approach to both the hardware and software components of the system. Addressing these aspects ensures the EHR system is not only functional but also efficient, secure, and poised to meet the evolving needs of modern healthcare.
Adhering to Security and Privacy Measures
Healthcare data breaches are a major concern, making security and privacy paramount in any EHR discussion. Investing in strong security measures protects your patients’ sensitive data and can save your healthcare facility from financial and reputation damage due to potential data breaches.
Your EHR vendors must adhere to the highest data security standards, but security measures within your organization are equally significant. Training staff about potential cyber threats, employing advanced encryption methods, and regular data backups can help create a robust defense against cyber-attacks.
Data Migration
Data migration is a vital step when adopting a new EHR system. It involves transferring existing records into the new system without data loss or corruption. An efficient data migration benefits patients and providers by ensuring a seamless transition without disrupting ongoing healthcare operations.
A detailed data migration plan should be developed before the actual migration. Considering the volume, types, and sensitivity of data to be migrated. Following the migration, periodic data audits should be carried out to ensure data accuracy and integrity.
Technical Expertise
Having skilled IT professionals as a part of your team can yield amazing benefits in EHR implementation and maintenance. These experts can handle system updates, troubleshoot technical issues, and provide necessary training to EHR users, thus ensuring smooth operation and minimizing downtime.
Ensuring a high ROI isn’t just about selecting the right EHR system but also having qualified staff to maintain and optimize it. In-house technical expertise or trusted partners can help surmount technical hurdles and keep your EHR system running at peak efficiency.
Conclusion
Maximizing EHR ROI is an ongoing journey that presents unique opportunities and challenges for healthcare providers. While this task may seem daunting, a strategic, carefully managed approach can improve patient care, operational efficiency, and ROI. Balancing upfront costs and ongoing expenses while reaping the benefits of enhanced healthcare delivery can position healthcare services for success in the long run. Remember, the key to achieving exceptional ROI lies in continuous refinement and the pursuit of excellence.